CONTACT US

SLT Long Pulse Nd: YAG Laser for the Treatment of Leg Veins and Benign Vascular Lesions
Constantin Confino, M.D., Dermatologist, Israel
Betty Czajkowsky, M.D., SharpLight Medical Advisor, Israel
Introduction
Laser treatment of superficial and deep leg veins as well as various other vascular lesions remains one of the more common applications of lasers in dermatology and phlebology. In fact, lasers have largely become the treatment of choice for vascular birthmarks such as hemangiomas and port-wine stains and the definitive treatment of rosacea. The range of congenital and acquired benign vascular lesions effectively treated with lasers continues to expand and is described by the principle of selective photothermolysis. In the case of vascular specific laser systems, the intended target is intravascular oxyhemoglobin.
By targeting oxyhemoglobin, energy is transferred to the surrounding vessel wall. Currently, the 1064-nm Nd: YAG laser and the visible/near infrared (IR) intense pulsed light (IPL) devices both give good results. The main difference, however, is that Nd: YAG lasers can penetrate much deeper and are therefore more suitable for the treatment of larger, deeper blood vessels such as leg veins. Another advantage of the Nd: YAG laser is its lower absorption coefficient for melanin. With a lower absorption coefficient for melanin, there is less concern for collateral epidermal damage so it may be more safely used to treat darker pigmented patients. The risk for post inflammatory hyper pigmentation can further be minimized by epidermal cooling devices. Epidermal cooling is imperative to safeguard against collateral damage from melanin absorption.
Leg vein therapy is one of the most commonly requested cosmetic procedures. Ecstatic venules present in approximately 40% of women and 15% of men. More than 70% have a family history. Often, pregnancy or other hormonal influences are implicated. Although a primarily cosmetic problem, more than half of these vessels may become symptomatic. The vascular network is a complex system of multiple vessels of different caliber and depths. Venous drainage of the leg consists of two primary channels, the deep muscular plexus and the superficial cutaneous plexus. The two channels are connected by deep perforating vessels. Smaller cutaneous vessels, which reside in the upper papillary dermis, drain to deeper reticular veins. The larger reticular veins dwell in the reticular dermis and subcutaneous fat. The superficial veins may be as large as 1 to2 mm. Reticular veins may be 4 to 6 mm in size. Larger veins have thicker walls, have a higher concentration of deoxygenated blood, and can be more than 4 mm deep. Variations in vessel size, depth, and oxygenation influence modality and efficacy of leg vein therapy. Visible light devices targeting the oxyhemoglobin absorption peaks may be acceptable for treating very superficial telangiectasias on the legs. Longer-wavelength, near-IR lasers allow deeper penetration of the tissue and may even be used to target deeper reticular veins. Longer wavelengths also heat more uniformly than the shorter wavelengths with higher absorption coefficients.
Laser leg vein treatment end points are immediate vessel disappearance or visible intravascular thrombosis or rupture. Microthrombi may be appreciable in the vessel lumen. Likewise, perivascular extravasations of blood may be apparent from vessel rupture. Occasionally, an audible pop may be appreciated with rupture. When very short pulse durations, less than 20 milliseconds, are used, spot sized purpura may occur. This is likely secondary to rapid microvascular heating and rupture.
The Nd: YAG modifications with variable spot sizes (1-6 mm) and higher fluences allow for focal vascular elimination with more limited collateral tissue damage. Clinical evaluation has shown that pulse durations between 40 and 60 milliseconds provide optimal treatment of leg veins.
The most common adverse side effect of laser treatment of leg veins is post inflammatory hyper pigmentation. This is seen more commonly with darker skin types, sun exposure, shorter pulse durations (<20 milliseconds), ruptured vessels, and vessels with thrombus formation. It fades with time, but this may be a year or longer in some cases. If excessive heating is delivered by either inappropriate fluence or pulse duration, ulceration and subsequent scarring may ensue.
Materials and methods
The new SLT long pulse Nd: YAG laser was tested on leg veins and various other vascular lesions. This laser emits up to 3 pulses per second at a fluencies of up to 450 J/cmA?, pulse duration of 10-100 msec and a spot size of 2 to 6 mm.
Proper eye protection for patient, physician and anyone else in the room is essential when using this laser.
External skin cooling and topical anesthesia is optional.
15 volunteer patients, 10 females and 5 males aged 35 to 55 years old were treated for leg veins and other vascular lesions.
In addition, one 10 years old girl was treated for PWS on the neck and one 15 years old girl was treated for a hemangioma on the neck.
Leg veins were treated once a month or after healing of previous treatment, for as many sessions as necessary (average 2-4 times).
Benign vascular lesions were treated twice.
In some cases it was necessary to use topical anesthesia and in all cases external air cooling was applied.
Photographs were taken before and after the treatments and one month after the last
treatment.
Results
| Very Satisfactory | Satisfactory | Not Satisfactory | |
| Superficial veins | 60% | 40% | 0% |
| Deep veins | 50% | 30% | 20% |
| Benign vascular Lesions | 80% | 20% | 0% |
The results were very satisfactory. Immediate skin reactions were redness and swelling, mild and transient. No severe or long term adverse effects were noticed.
Patients' and practitioner's satisfaction grade was high (80%).
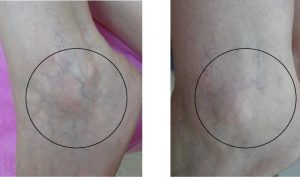
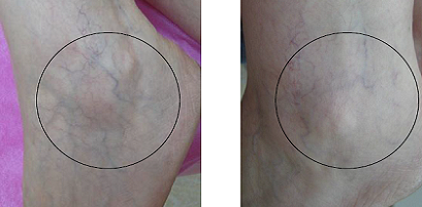
B/A photos
1 month after 1 Leg veins treatment
Conclusions
As our understanding of superficial and deep leg veins and congenital and/or acquired benign vascular lesions removal continues to grow and laser technology continues to evolve, we will move further toward the goal of achieving rapid lesion clearance with minimal risk and low morbidity.
This study confirms the safety and efficacy of the new SLT long pulse Nd: YAG laser for these applications and is inline with previously published reports on long pulse vascular lasers. Good final results with the minimum side or adverse effects were achieved. Patients' and practitioner's satisfaction grade was high.
References
1. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 1983; 220:524- 7.\
2. Dixon J, Huether S, Rotering RH. Hypertrophic scarring in argon laser treatment of portwine stains. Plast Reconstr Surg 1984;73:771 – 80.
3. Apfelberg DB, Maser MR, Lash H, Rivers J. The argon laser for cutaneous lesions. JAMA 1981;245:2073 – 5.
4. Arndt KA. Argon laser therapy of small cutaneous benign vascular lesions. Arch Dermatol 1982;118:200 – 24. Fig. 10 (A) Leg vein prior to treatment with laser. (B) Post inflammatory hyperpigmentation 2 mo. following laser treatment. D. 14 Railan et al.
5. Geronemus RG. Argon laser for the treatment of cutaneous lesions. Clin Dermatol 1995;13:55- 8.
6. Apfelberg DR. Argon-pumped tunable dye laser. Ann Plast Surg1994;32:394 – 400.
7. Thibault PK. A patient's questionnaire evaluation of krypton laser treatment of facial telangiectases: a comparison with the copper vapor laser. Dermatol Surg 1997;23:37 – 41.
8. Dinehart SM, Warner M, Flock S. The copper vapor laser for treatment of cutaneous vascular and pigmented lesions. J Dermatol Surg Oncol1993;19:370 -5.
9. Goldberg DJ, Meine JG. A comparison of four frequency-doubled:YAG (532 nm) laser systems for treatment of facial telangiectasias Nd Dermatol Surg 1999;25:463
10. Levine VJ, Geronemus RG. Adverse effects associated with the 577- and 585- nanometer pulsed dye laser in the treatment of cutaneous benign vascular lesions: a study of 500 patients. J Am Acad Dermatol 1995; 32:613 – 7.
11. Garden JM, Polla LL, Tan OT. The treatment of port wine stains by the pulsed dye laser: analysis of pulse duration and long-term therapy. Arch Dermatol 1998;124:889 –96.
12. Tan OT, Sherwood K, Gilchrest BA. Treatment of children with portwine stains using the flashlamp-pumped pulsed dye laser. N Engl J Med 1989;320:416- 21.
13. Alster TS, Wilson F. Treatment of port-wine stains with the flashlamppumped pulsed dye laser. Ann Plast Surg 1994;32:478- 84.
14. Fitzpatrick RE, Lowe NJ, Goldman MP, et al. Flashlamp-pumped pulsed dye laser treatment of port-wine stains. J Dermatol Surg Oncol1994;20:743- 8.
15. Sommer S, Sheehan-Dave RA. Pulsed dye laser treatment of port-wine stains in pigmented skin. J Am Acad Dermatol 2000;42:667- 71
16. Chang C, Nelson JS. Cryogen spray cooling and higher fluence pulsed dye laser treatment improve port-wine stain clearance while minimizing epidermal damage. Dermatol Surg 1999;25:767 – 72.
17. Waldorf HA, Alster TS, McMillan K, et al. Effect of dynamic cooling on 585-nm pulsed dye laser treatment of port-wine stain birthmarks Dermatol Surg 1997;23:657- 62.
18. Renfro L, Geronemus RG. Anatomical differences of port-wine tains in response to treatment with the pulsed dye laser. Arch Dermatol 1993; 129:182- 8
19. Lou WW, Geronemus RG. Treatment of port-wine stains by variable pulsed width pulsed dye laser with cryogen spray: a preliminary study. Dermatol Surg 2001;27:963- 5.
20. Dierickx CC, Casparian JM, Vengopalan V, Farinelli WA, Anderson RR. Thermal relaxation of port-wine stain vessels probed in vivo: the need for 1-10 millisecond laser pulse treatment. J Invest Dermatol1995;105:709- 14.
21. Uebelhoer NS, Bogle MA, Dover JS, Rohrer TE, Arndt KA. Comparison of KTP (532nm Gemini) with pulsed dye laser (595nm, V-Beam) in the treatment of facial telangiectasia and redness. Unpublished data.
22. No D, Dierickx C, McClaren M, et al. Pulsed alexandrite treatment ofbulky vascular malformations. Lasers Surg Med 2003;15:26.
23. Rogachefsky AS, Silapunt S, Goldberg DJ. Nd:YAG laser (1064nm) irradiation for lower extremity telangiectases and small reticular veins: efficacy as measured by vessel color size. Dermatol Surg 2002; 28:220 – 3.
24. Ross EV, Domankevitz Y. Laser treatment of leg veins: physical mechanisms and theoretical considerations. Lasers Surg Med 2005; 36:105-16.
25. Yang MU, Yaroslavsky AN, Farinelli WA, et al. Long pulsed Nd:YAG treatment for port wine stains. Lasers Surg Med 2003;15:28.
26. Parlette EC, Groff WF, Kinshella MJ, Domankevitz Y, Ross EV. Optimal pulse durations for the treatment of leg telangiectasias with a neodymium YAG laser. Lasers Surg Med 2006 [in press].
27. Raulin C, Schroeter CA, Weiss RA, Keiner M, Werner S. Treatment of port-wine stains with a noncoherent pulsed light source. Arch Dermatol 1999;135:679- 83.
28. Raulin C, Hellwig S, Schonermark MP, et al. Treatment of a nonresponding port-wine stain with a new pulsed source (Photoderm VL). Lasers Surg Med 1997;21:203
29. Palomar Medical. Handpieces and accessories. Web address: www.palomarmedical.com.
30. Rohrer TE, Chatrath V, Iyengar V. Does pulse stacking improve results with variablepulse pulsed dye lasers? Dermatol Surg 2004;30:163- 7.
31. Iyer S, Fitzpatrick RE. Long-pulsed dye laser treatment for facial telangiectasias and erythema: evaluation of a single purpuric pass versus multiple subpurpuric passes. Dermatol Surg 2005;31:898- 902.
32. Anderson RR, Ross EV. Laser-tissue interactions. In: Fitzpatrick MP, Goldman MP, editors. Cosmetic laser surgery. St Louis (Mo)7 Mosby; 2000.
33. Butler EG, McClellan SD, Ross EV. Split face treatment of photodamaged skin with a 10 mm spot KTP laser vs IPL: a cheek-to-cheek comparison. Lasers Surg Med 2005;78(36 Suppl):256.
34. Negishi K, Kushikata N, Tezuka Y, et al. Study of the incidence and nature of bvery subtle epidermal melasmaQ in relation to intense pulsed light treatment. Dermatol Surg 2004;30:881 -6.
35. Negishi K, Tezuka Y, Kushikata N, Wakamatsu S. Photorejuvenation for Asian skin by intense pulsed light. Dermatol Surg 2001;27:627- 32.